![]()
Can there be Sickle Cell Disease when I am sickling negative?
Dear George, Your situation is a frequent occurrence at the clinic. You were emphatic that she is AS but you are sickling negative. That doesn't mean that all your haemoglobins are normal.
Advertisement
There are situations where somebody has inherited one normal haemoglobin and one abnormal haemoglobin from the parents but the conventional sickling test done will be negative.
This is because the abnormal haemoglobins C and F do not sickle when tested with the sickling test. Thus, one can be AC or AF and still test negative to the sickling test alone.
However, an HB electrophoresis test will identify the exact combinations. It is for this reason that one must never stop at just the sickling test in an attempt to find out his sickle cell status.
The HB electrophoresis test MUST always be done even if the sickling test is negative. In your situation, your electrophoresis may well show that you are AF.
For somebody to have SCD, there must be the presence of two abnormal haemoglobins, one of which must be haemoglobin S. By this reasoning, a person with one haemoglobin S and haemoglobin F, which is foetal haemoglobin, is also considered as suffering from SCD.
The same goes for those with haemoglobin combinations as SC, SBthal etc. So far as there is one S as part of the abnormal haemoglobin combinations, there is SCD. By this reasoning then, CC and FF combinations are not sickle cell disease even though there are two abnormal haemoglobin combinations.
Foetal hemoglobin, as the name implies, is the main transporter of oxygen in the human foetus during the last seven months of development in the womb. This haemoglobin persists in the newborn until about six months of age after birth.
Additionally, foetal haemoglobin is different from adult haemoglobin, in that it is able to take up oxygen with greater affinity than the adult form, giving the developing foetus better access to oxygen from the mother's bloodstream.
Foetal haemoglobin gets replaced completely by adult haemoglobin around six months after birth. When foetal haemoglobin production is switched off after birth, normal children begin producing adult haemoglobin.
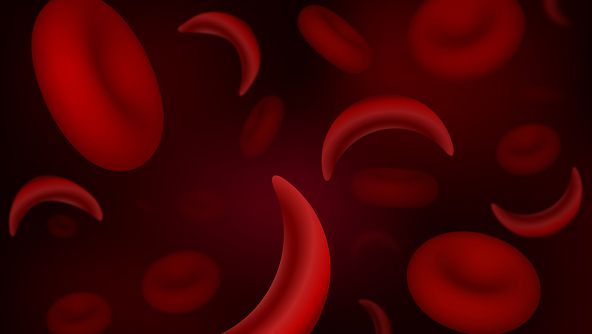
Children with SCD instead produce haemoglobin S, which aggregates together and forms crystals that cause red blood cells to change their shape from round to sickle-shaped.
These defective red blood cells have a greater tendency to get stuck on top of one another and block blood vessels. These lead to painful vaso-occlusive episodes which characterise the disease.
If foetal haemoglobin remains the predominant form of haemoglobin after birth, the number of painful episodes decreases in patients with SCD. The foetal haemoglobin's reduction in the severity of the disease comes from its ability to inhibit the formation of haemoglobin aggregates within red blood cells which also contain haemoglobin S.
Foetal haemoglobin is desirable, not only because of its greater affinity for binding oxygen but it does not sickle and hence not destroyed easily. Besides, foetal haemoglobin production can be reactivated by medications such as hydroxyurea.
Hydroxyurea promotes the production of foetal haemoglobin and can, thus, be used to treat SCD. Combination therapy with hydroxyurea and recombinant erythropoietin has been shown to further elevate haemoglobin F levels.
Foetal haemoglobin's affinity for oxygen is substantially greater than that of adult haemoglobin. This greater affinity for oxygen is explained by the lack of interaction with a particular substance that decreases the affinity for oxygen in the red blood cells.
This enables the foetal haemoglobin to extract oxygen from the maternal blood across the placenta.
Certain genetic abnormalities can cause the switch to adult haemoglobin synthesis to fail, resulting in a condition known as hereditary persistence of foetal haemoglobin.
Increasing the body's production of foetal haemoglobin is used as a strategy to treat SCD. It stands to reason, therefore, that people with SF genotype of SCD will get a milder form of the disease compared to those with SS and SC genotypes.
In addition, the SF genotype is known to be able to withstand better certain stressors such as an oxidative stress manifesting as reduced episodes of crises.
However, the symptoms akin to the other types of SCD apply to those with SF genotype. Vasocclusive crisis, hyperhemolytic crisis, aplastic crisis and all the other symptoms that characterise other sickle cell genotypes apply here too.
Folic acid, multivitamins, vitamin C, three-six monthly dewormers, as well as regular reviews by a specialist in the field of SCD will suffice.
All the other precautions that patients with SCD exercise must also be strictly adhered to.
[email protected]. A member of Paediatric Society of Ghana.