The health impact of COVID-19 on other medical conditions in Ghana – the opinion of a kidney specialist and health equity specialist
The COVID-19 pandemic has changed the world with devastating effects. Most countries have declared lockdowns in various forms at different times as a way to curb the spread of this novel Coronavirus. The lifestyles of people have generally changed with great economic and social burden.
Terminologies like physical distancing, frequent handwashing, use of hand sanitizers, use of face masks, quarantine, self-isolation, etc have dominated our speeches.
Advertisement
The rate of spread of the virus is astronomical with an increasing death rate. As of 3rd June, 2020 there were 6,523,137 documented cases with 385,015 deaths and 3,104,281 full recoveries according to John Hopkins University since the outbreak in Wuhan in December 2019.
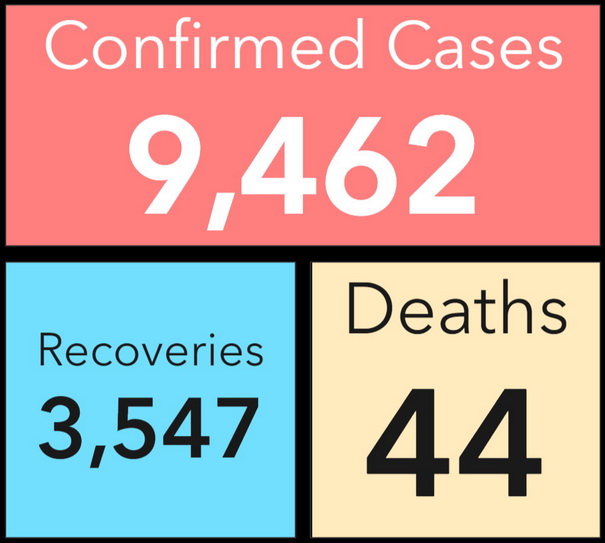
In Ghana, we currently have 9,462 confirmed cases with 44 deaths and 3,547 recoveries according to the Ghana Health Service. Ghana, just like most African countries, has low infectivity and mortality rates as compared to the rest of the world. There are suggestions that the climate, younger population, some genetic advantages (unproven) as well as low testing are accounting for the low reported infectivity rates in Africa. But as this has been consistent for a while, low testing may not necessarily be a confounder as previously thought.
As a Senior Physician Specialist and nephrologist in one of the largest teaching hospitals in Ghana, in my opinion, though COVID-19 is devastating, it is possible that we are losing more lives in Ghana to other medical conditions from the COVID-19-induced restrictions and phobias.
I believe that more lives are being lost to other communicable diseases such as meningitis which kills more people in a short period than COVID-19 but not getting the media attention and support it deserves. The case fatality rate for COVID-19 globally is 5.9% and only 0.42% in Ghana according to John Hopkins University data.
The case fatality rate of COVID-19 is far lower than the case fatality rate of meningitis for example, where at least 409 recorded cases in five regions in the Northern sector of the country resulted in 40 deaths as of Wednesday April 15, representing a 15% case fatality rate according the Ghana Health Service.
Generally, there may be neglect of other non-communicable diseases such as diabetes, hypertension and chronic kidney disease leading to devastating complications such as stroke, heart failure and heart attacks with high morbidity and mortality in this COVID-19 pandemic.
Why am I bothered? I think the restrictions and protocols set in our hospitals affect the clinical management of patients who present with other conditions with symptoms similar to COVID-19. By the COVID-19 screening protocols, most patients who report with symptoms meeting the criteria for COVID-19, are isolated and managed until the COVID-19 test results are in. It normally takes between three to seven days to get test results.
The problem with the protocol is that isolated patients may not get access to appropriate specialist services as there aren’t adequate personal protective equipment for the specialists to manage patients appropriately. The specialists may not review such patients leading to poor management which may result in death. Again, those who are not infected are at risk of infection whilst waiting in isolation with potentially infected COVID-19 patients.
In Ghana, we were on partial lockdown at a point. During the partial lockdown people were asked to stay home and come out only for essential services such as food and healthcare. Public transport was not available and most clinics had also shut down their outpatients’ clinics and were running only emergencies. With the shutdown of outpatient’s clinics, most people who had to come in for appointments and refill their chronic medications were not able to do so. These patients are now coming in very sick with very high blood pressures and high blood sugars with devastating complications as a result of the running out of their chronic medications. Some come in very sick on admission and unfortunately will have to be in isolation for some days pending test results with variable outcomes.
A case in question was when a 45-year-old patient with diabetes and hypertension who came in with a chest infection (pneumonia) and COVID-19 justifiably had to be ruled out. He was kept in isolation for about a week pending his test results during which he was sub optimally treated. By the time his test came back negative, he had deteriorated, as he was not getting the best of care in the holding area and unfortunately died from severe infections after a few days with kidney injury.
My question is, could this gentleman have survived this predicament if he had been reviewed by specialists from day one? Would he have died if there was no COVID-19 to worry about? Your guess is as good as mine.
During the lockdown to curb the spread of COVID-19, what will a patient with kidney failure who is expected to come to the hospital for dialysis three times a week do? How can he get public transport to the dialysis centre if he does not own a car? How can he manage to get through all the barriers and convince the military men that he needs to come to the hospital for his dialysis sessions?
Some passengers were prevented from getting into the city by buses. Drivers of mini-buses were sometimes asked to let their passengers alight at a point and walk for the rest of the journey in some parts of the city. How could a patient with kidney failure on dialysis walk such distances? Would they not get breathless on coming into the hospital and be isolated and screened as suspected COVID-19 cases and hence denied dialysis with complications?
During the lockdown most people on daily wages ran out of money, some people also lost their jobs. The socio-economic impact of COVID-19 on low and middle income countries is phenomenal. The already low economy was virtually grinding to a halt. Many people ran into financial difficulties and some were not able to purchase their chronic medications. The government of Ghana had to ease restrictions at a point because of public agitation out of poverty and hunger as the feeding of vulnerable groups was costing the nation about two million Ghana Cedis (357,142 US dollars) a day, according to the National Disaster Management Organisation (NADMO).
The feeding created problems as people were refusing to adhere to the physical distancing protocols in some communities. I know some philanthropic organizations that had to stop sharing food in a particular community because they were rather increasing the risk of spread as the people were pushing and shoving each other to get their daily bread against government directives.
The poor and the marginalized were the hard hit with no food, no transport and limited access to healthcare when needed. These could have led to unrecorded deaths or morbidities. The story of forty head porters in Accra who were smuggling themselves in a cargo truck back to their hometown made the news when they were forced to return. They were starving in the cities with no work to do and could not feed themselves and their children. This would lead to malnutrition and predispose them to infections.
In our hospitals there are inadequate personal protective equipment. This makes clinicians afraid to examine patients properly. How can the right diagnosis be made if clinicians are afraid to get close to patients for fear of COVID-19. As clinicians, we know that there are many causes of fever, cough or shortness of breath aside COVID-19. These causes are more common than COVID-19. However, currently, patients are left to their fate for fear of having COVID-19 until the test comes negative with detrimental consequences in some cases.
There were directives at a point for clinicians to examine only when extremely necessary to prevent exposure to COVID-19 and I guess we might miss some important diagnosis as a result of the fear for COVID-19. Unfortunately, if patients come with comorbidities and die with a positive COVID-19 test, it will be recorded as having died from COVID-19. The question however is, did the patient die from some other medical complication with COVID-19 or died directly from COVID-19? It’s not surprising that those dying have underlying conditions and I will not be surprised if the cause of death in some of these patients is from the poor management of the underlying condition and not COVID-19.
Again, during the COVID-19 period some institutions had staff coming in shifts to decrease risk of exposure and also ensure physical distancing. This ends up decreasing the quality of care as a result of the decreased human resource.
Some laboratories were also not running at full capacity and some private laboratories who send samples outside the country could not do so as a result of border closures. This affects diagnosis and management. I believe some patients may have lost their lives as a result of mismanagement during this period indirectly from COVID-19 restrictions. As a nephrologist managing kidney transplant patients where regular checking of their drug levels is mandatory, there is a potential for patients to lose their kidneys. The closure of the borders also made it difficult for some transplant patients to access imported medications thus potentially increasing the risk of kidney rejection.
In conclusion, COVID-19 is a highly infectious disease with generally lower infectivity rate and mortality in Ghana. Measures put in place to curb the spread should not be detrimental to patients suffering from other medical conditions with higher case fatality in Ghana. Heads of institutions and the Ministry of Health should make personal protective equipment available for healthcare workers to provide the best care for patients to prevent unnecessary deaths from other medical conditions as a result of phobia from COVID-19. Until then I ask, are we losing more lives to other medical conditions as a result of fear for COVID-19 which arguably has a lower mortality rate?
Thank You
Dr. Elliot Koranteng Tannor
Senior Specialist Physician/Nephrologist
Senior Atlantic Fellow for Health Equity



